In This Section:
- About The Knee
- Meniscus injuries (knee arthroscopy)
- ACL reconstruction
- Patient Matched knee replacement surgery
About The Knee
Your knee is a complex joint with many components, making it vulnerable to a variety of injuries.
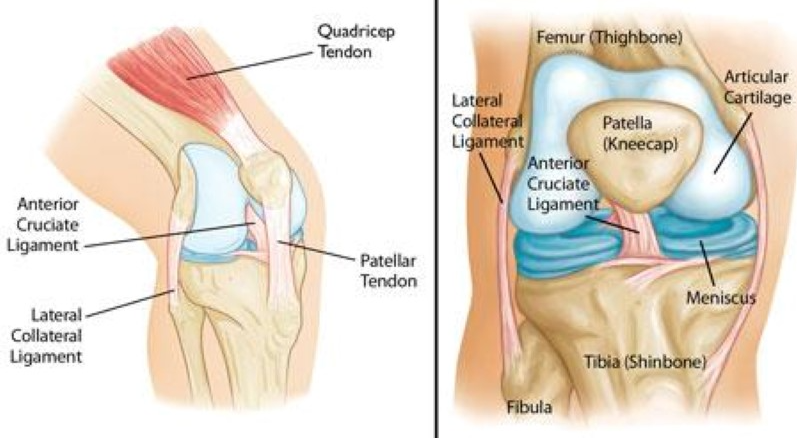
Three bones meet to form your knee joint: your thighbone (femur), shinbone (tibia) and kneecap (patella). Your kneecap sits in front of the joint to provide some protection.
Bones are connected to other bones by ligaments. There are four primary ligaments in in your knee. They act like strong ropes to hold the bones together and keep your knee stable.
The femur and tibia and the back of the patella are covered the articular cartilage. This slippery substance helps your knee bones glide smoothly across each other as you bend and straighten your knee.
Two wedge-shaped pieces of meniscal cartilage act as ‘shock absorbers’, between your femur and tibia. Unlike the articular cartilage, the meniscus is tough and rubbery to help cushion and stabilise the joint. When people tale about torn cartilage in the knee they are usually referring to a torn meniscus.
Collateral ligaments are found on the sides of your knee. The medial collateral ligament is on the inside and the lateral collateral ligament is on the outside. They control the sideways motion of your knee and brace it against unusual movement.
Cruciate ligaments are also found on the inside of your knee. They cross each other to form an “X” with the anterior cruciate ligament in the front and the posterior cruciate ligament in the back. The anterior cruciate ligament (ACL) runs diagonally in the middle of the knee. It prevents the tibia sliding out in front of the femur, as well as provides rotational stability to the knee.
Knee injuries
Pain and swelling are the most common signs of knee injury. In many cases injuries involve more than one structure in the knee. The severity of the joint pain can will vary depending on which structure is involved, from a minor ache to a severe and disabling pain.
Meniscus injuries
The menisci (medial and lateral) are made of cartilage and act as shock absorbers between the bones in the knees. Our cartilages become a little brittle as we get older and therefore can tear a little easier. Twisting type injuries caused from a sporting injury (acute trauma) or even by a simple twisting injury such as arising from a squatting position or getting out of a chair can cause discomfort.
Symptoms
- Pain over the torn area i.e. inner or outer side of the knee
- Redness and swelling
- Reduced motion ie the inability to extend the knee
- Locking of the knee (unable to bend the knee) if the cartilage gets caught between the femur a tibia
- Limping due to discomfort
- Difficulty weight bearing or walking
- The sensation of your knee ‘giving way’
Examination
Dr Savvoulidis will discuss your symptoms and medical history, conduct a physical examination, and review your x-rays.
He will assess –
- Your tenderness and structures around the injured knee and compare them to the uninjured knee.
- Check for signs of injury to the muscles, tendons, and other ligaments surrounding the knee.
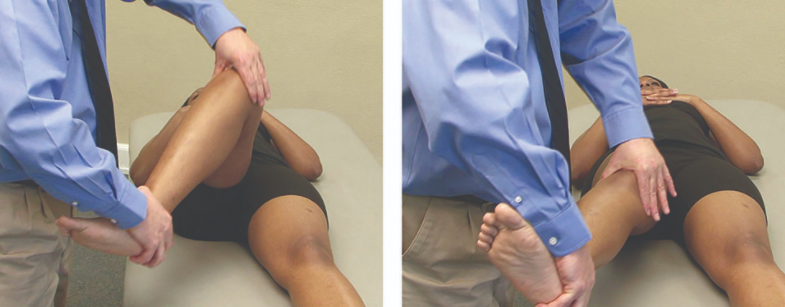
- Perform a McMurray Test. Dr Savvoulidis will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement may cause pain, clicking or a clunking sensation within the joint.
- Order an MRI to make the diagnosis of a torn ACL, x-rays will only show whether there injury is associated with a broken bone.
Conservative Management
Many meniscal tears will not need immediate surgery. If your symptoms do not persist and you have no locking or swelling of the knee, Dr Savvoulidis may recommend nonsurgical treatment.
- Rest, Ice, Compression and Elevation
- Non-steroidal anti-inflammatory medications
- Steroid injection into your knee joint may help eliminate pain and swelling.
- Platelet Rich Plasma (PRP) injections. The platelets in your blood contain growth factors. Dr Savvoulidis will discuss this as an option. It is believed that injecting PRP growth factors from your own blood into an injured area will help tissues repair themselves by causing new cells to form.
Surgical Treatment
If your symptoms persist with conservative treatment, Dr Savvoulidis may suggest arthroscopic surgery.
It is standard to remove only the torn section of cartilage, ideally the knee should recover and become symptom free. If the entire meniscus is removed, the knee will develop osteoarthritis in 15 to 20 years.
Knee Arthroscopy
Knee arthroscopy is performed by inserting a special instrument called an arthroscope into your knee through a small incision (portal). A fiber-optic camera (is attached to the arthroscope) that provides a clear view of inside the knee. These images are seen on a television screen (monitor). Dr Savvoulidis uses it to see inside the joint to evaluate and treat various conditions. Dr Savvoulidis will then insert miniature surgical instruments through two or three other small portals to trim or repair the tear.
Using this technique Dr Savvoulidis can repair many of the injuries, and if required remove small pieces of loose bones or cartilage during this procedure.
Knee arthroscopy is common surgical procedure and is generally performed as day surgery and is usually done under general anaesthesia.
You will be given post-operative advice and exercises to perform prior to surgery and will be reviewed two weeks following your surgery.
ACL Reconstruction
A rupture of the anterior cruciate ligament (ACL) is common in sporting injuries. The ACL can be injured in several ways:
- Due to a sudden stop and change in direction.
- Slowing down while running.
- Landing from a jump incorrectly.
- Direct contact or collision, such as a football tackle.
When you injure your ACL, you might hear a “popping” noise and you may feel your knee give way from under you.
Symptoms
- Pain with swelling.
- Loss of full range of motion.
- Tenderness along the joint line.
- Discomfort while walking.
Injuries of the ACL are distressing for younger athletic people. Once ruptured the ACL does not heal and usually causes instability of knee and the inability to return to normal sporting activities.
Examination
Dr Savvoulidis will discuss your symptoms and medical history, conduct a physical examination, and review your x-rays.
He will assess –
- Your tenderness and structures around the injured knee and compare them to the uninjured knee.
- Range of motion both – passive (assisted) and active (self-directed).
- Check for signs of injury to the muscles, tendons, and other ligaments surrounding the knee.
- Order an MRI to make the diagnosis of a torn ACL, x-rays will only show whether there injury is associated with a broken bone.
Conservative Treatment
A torn ACL will not heal without surgery. For patients who are elderly or have a very low activity level conservative management may suffice.
Bracing – it may be appropriate to wear a brace to protect your knee from instability.
Physiotherapy – as the swelling goes down, a specific rehabilitation program aimed a restoring function to your knee and strengthening the leg muscles that support it may be initiated.
Surgical Treatment
Most ACL tears cannot be stitched (sutured) back together. To surgically repair the ACL and restore knee stability, the ligament must be reconstructed.
Reconstructive surgery means that the old ACL is removed, and a new ligament created. The most common locations to harvest tissue graft are from the patellar tendon in the front of the knee or the hamstring tendon in the back of the thigh. A new ligament is shaped to replace the ruptured ligament. It is inserted in the location of the normal ACL and held in place with a fixation device. This procedure is performed using arthroscopic surgery. Once this has healed it assumes the role of a normal anterior cruciate ligament.
Even with successful reconstructive surgery, because regrowth takes time, there is a long recovery period. You will be given a specific rehabilitation program to follow under guidance and advice from your physiotherapist.
The most important goal is to ensure the best chance of long-term recovery and return to sports activities, is with the structured rehab program, and not the speed with which you progress through your rehabilitation.
Lastly, we know that people who undergo ACL reconstructive surgery have a much higher chance of developing osteoarthritis of the knee joint, and often this occurs in the decades following ACL reconstruction.
Patient Matched Knee Replacement Surgery
The knee joint is the largest joint in the body. It is known as the “hinge” joint that allows the knee to flex, extend and rotate. It is formed by the tibia (shin bone), the femur (thigh bone), and the patella (knee cap). It is surrounded and held together by muscles, ligaments and other soft tissues. Each bone end is covered with a layer of joint cartilage that cushions the knee and allows smooth movement of the joint.
Osteoarthritis is the most frequent form of arthritis which is responsible for people undergoing knee replacement surgery. Osteoarthritis is the progressive wearing of the bearing surface of the knee joint. The cartilage becomes soft and frayed and eventually is worn away and leaves the underlying bones exposed. As the disease progresses, pain and stiffness usually occur, mobility decreases and quality of life becomes affected.
A total knee replacement is where the damaged areas of the knee and cartilage are removed and replaced with metallic and plastic components.
The outcomes following surgery are generally good. You will notice a decrease in your pain, increased mobility and improvement of your general lifestyle.
Complications
Total knee replacement is a complex surgical procedure. Most patients experience no particular problems with the surgery but it is inevitable that with major surgery, there are some risks and
you should be aware of them. Dr Savvoulidis would have discussed this with you when you signed your surgical consent. Do however remember that this operation is designed to improve your
quality of life and is usually only undertaken when all other avenues of treatment have failed and the benefits outweigh the risks.
Complications include:
- Blood clots: This is a possible complication following joint replacement surgery. Generally blood clots form in the calf muscle. This risk of this is reduced by early mobilisation and blood thinning medication. You will have a scan of your legs 2 weeks after your operation to see if you have had any clots form. Many clots found, are superficial and as you are discharged on Aspirin no further intervention is usually taken.
- Embolism: Occasionally clots or fatty material can go to the lungs leading to severe breathing difficulty or even death.
- Infection: Fortunately, good surgical technique and the use of antibiotics reduce this complication. However, if it does occur, it is serious and may result in the need to remove the artificial joint components.
- Loosening: This could occur after 10 to 15 years. Occasionally, the knee will loosen earlier.
- Blood loss: It is common to lose blood during the operation. It is a complication of any surgery and will be treated as needed.
- Neurovascular complication: There are many major blood vessels and nerves situated around the joint which in rare cases may be damaged during the operation.
- Mobilisation: A limp is common for a number of weeks or months following your operation but usually improves with time and exercises.
- Leg Length Discrepancy: Sometimes this can occur but can be corrected with the use of a heel raise in your shoe.
Follow Up
You will continue to be reviewed at regular intervals following your joint replacement surgery. You will require xrays prior to all appointments. At the time of booking your surgery you will be given forms to have a post operative scan at 2 weeks, an xray form to have done at 5 weeks post surgery and an appointment for a post operative consultation at 6 weeks. It is important that you
keep these appointments. If you need to change the date or time, please contact Dr Savvoulidis’ rooms.
Please view our frequently asked questions under the FAQ section.
