In This Section:
- Osteoarthritis of the hip
- Anterior Minimally Invasive Hip Replacement (Arthroplasty)
- Labral Tears
- Hip Arthroscopy
Osteoarthritis of the Hip
General
Bones provide a frame to keep the body supported and protect various organs. They enable movement to occur, serve as an attachment point for skeletal muscles, tendons, and ligaments, and connect via joints.
The musculoskeletal system is responsible for every movement an individual makes. When something goes wrong with the musculoskeletal system, an individual’s range of motion or ability to move can be impacted.
How a normal hip works
The hip joint is a ball-and-socket joint. This type of joint with a ball shaped bone fitting into a cup like socket permits the joint to move in a circle. The surfaces of the ball and socket are covered with articular cartilage, a smooth, slippery substance that covers the surface of the bones to protect them, reduce friction and ease movement. The surface of the joint is covered by a thin lining called the synovium. The synovium produces a small amount of fluid that lubricates the cartilage and aids in movement.
Physical changes that occur in an osteoarthritic hip
Osteoarthritis of the hip joint occurs when wear and tear on the joint causes this smooth surface to gradually wear away over time. As the bones rub directly against each other they can be damaged and small growths called bone spurs (osteophytes) can develop.
These changes can cause pain, stiffness, and difficulty in moving and limit the hip joints range of motion.
It can make it hard to do everyday activities like bending over to tie a shoelace, rising from a chair, or taking a short walk.
The risk of getting osteoarthritis increase with age. Those that have played a lot of sport, or performed heavy manual work are prone to the disease.
Symptoms
- Stiffness may be worse in the morning, or after sitting or resting for a while. Over time, painful symptoms may occur more frequently, including during rest or at night.
- Pain in your groin or thigh that radiates to your buttocks or your knee.
- Pain that flares up with vigorous activity
- Stiffness in the hip joint that makes it difficult to walk or bend.
- “Locking” or “sticking” of the joint, and a grinding noise (crepitus) during movement caused by loose fragments of cartilage and other tissue interfering with the smooth motion of the hip.
- Decreased range of motion in the hip that affects the ability to walk and may cause a limp.
If you become inactive so that you do not experience the pain, your muscles which surround the hip will become weak. This can lead to a greater risk of falling.
Examination
Dr Savvoulidis will discuss your symptoms and medical history, conduct a physical examination, and review your x-rays.
He will assess –
- Your tenderness around the hip.
- Range of motion both – passive (assisted) and active (self-directed).
- Crepitus (grating sensation inside the joint) with movement.
- Pain when pressure is placed on the hip.
- Problems with your gait (the way you walk).
- Any signs of injury to the muscles, tendons, and ligaments surrounding the hip.
Conservative Treatment
Depending on the degree of the disease you can maintain the osteoarthritis conservatively by
- Resting your hip and only doing mild exercise like walking or swimming. Avoid exercise that will cause you greater pain. Rest after you have exercised.
- Watch your diet and your weight. Being overweight will put more stress on your hip and cause you more pain.
- Get enough sleep at night.
- Use Panadol and non-steroidal anti-inflammatory medicines like Ibuprofen.
- You may need a walking stick should a limp develop, and your hip become painful.
- Wear good supporting shoes.
- Physiotherapy or water aerobics may help to keep your hip functioning and improve its strength and range of movement.
- Always consult your Doctor before you embark on any exercise or before you take any medication.
Surgical Treatment
If you have later stages of osteoarthritis, your hip joint hurts when you rest at night, and / or your hip is severely deformed, Dr Savvoulidis may recommend total hip replacement surgery (arthroplasty).
Anterior Minimally Invasive Hip Replacement
Up walking hours after surgery with little pain and a return to a normal lifestyle within weeks is now possible following hip replacement surgery. The traditional posterior approach to the hip cuts, splits or detaches major muscles about the joint that are essential for normal gait. It is performed via a 20 – 30cm posterior incision. It is this muscle damage that is the cause of most of the post operative pain and difficulty in rehabilitation following a total hip replacement.
Gait Analysis and MRI studies have shown that permanent muscle damage caused by traditional approaches in hip replacement surgery results in most cases of long term limp and instability problems such as dislocation. This can be avoided by an Anterior Minimally Invasive Approach.
Minimally Invasive Surgery is the most important revolution in surgical technique since the early 1900s. The anterior approach to the hip is a well described technique that has been in common usage for over 70 years.
For Total Hip Replacement to be considered truly minimally invasive it must:
- Not divide, detach or split any muscles.
- Approach the joint via an inter-nervous plane.
- Be achievable via a small (6 – 8cm) cosmetic incision.
- Result in less post-operative pain, fewer complications and a quicker rehabilitation.
- These criteria are only possible via an anterior minimally invasive approach.
Less Pain – Rapid Rehabilitation
The AMIS technique approaches the hip joint from the front via a small 6 – 8cm incision. This avoids the major muscles of the buttock which are cut during a traditional approach.
No muscles or tendons are cut in the anterior approach resulting in less post-operative pain, fewer complications, shorter hospital stay and a more rapid rehabilitation resulting in better functional results with a greater improvement in quality of life. Patients are able to mobilise fully weight bearing on the day of surgery and may progress to a single walking stick by the time of discharge from hospital on day 3 or 4. Patients are able to return to normal daily activities and recreational sports much earlier than with other conventional approaches.
Complications
Total hip replacement is a complex surgical procedure. Most patients experience no particular problems with the surgery but it is inevitable that with major surgery, there are some risks and you should be aware of them. Dr Savvoulidis would have discussed this with you when you signed your surgical consent. Do however remember that this operation is designed to improve your quality of life and is usually only undertaken when all other avenues of treatment have failed and the benefits outweigh the risks.
Complications include:
- Blood clots: This is a possible complication following joint replacement surgery. Generally blood clots form in the calf muscle. This risk of this is reduced by early mobilisation and blood thinning medication. You will have a scan of your legs 2 weeks after your operation to see if you have had any clots form. Many clots found, are superficial and as you are discharged on Aspirin no further intervention is usually taken.
- Embolism: Occasionally clots or fatty material can go to the lungs leading to severe breathing difficulty or even death.
- Infection: Fortunately, good surgical technique and the use of antibiotics reduce this complication. However, if it does occur, it is serious and may result in the need to remove the artificial joint components.
- Loosening: This could occur after 10 to 15 years. Occasionally, the hip will loosen earlier.
- Blood loss: It is common to lose blood during the operation. It is a complication of any surgery and will be treated as needed.
- Neurovascular complication: There are many major blood vessels and nerves situated around the joint which in rare cases may be damaged during the operation.
- Mobilisation: A limp is common for a number of weeks or months following your operation but usually improves with time and exercises.
- Leg Length Discrepancy: Sometimes this can occur but can be corrected with the use of a heel raise in your shoe.
Follow Up
You will continue to be reviewed at regular intervals following your joint replacement surgery. You will require xrays prior to all appointments. At the time of booking your surgery you will be given forms to have a post operative scan at 2 weeks, an xray form to have done at 5 weeks post surgery and an appointment for a post operative consultation at 6 weeks. It is important that you keep these appointments. If you need to change the date or time, please contact Dr Savvoulidis’ rooms.
Please view our frequently asked questions under the FAQ section.
Labral Tears
The labrum is a ring of cartilage that follows the outside rim of your hip joint. It cushions the hip joint and helps hold the ball of the top of your thighbone securely within your hip joint. The connective tissue can tear or detach from the bone, causing discomfort and restricted motion.
A hip labral tear is a common injury that may cause hip and groin pain as well as other symptoms such as:
- Clicking or hip locking sensation in the hip area (this may get worse when you move, bend, or rotate the hip, depending on the severity and location of the tear)
- Hip pain or stiffness – this can be made worse by long periods of standing, sitting, or walking.
- Pain in the groin or buttocks area
- Feeling unsteady on your feet
- Limited range of motion in your hip joint
You may have a hip labral tear with no symptoms at all.
Causes of hip labral tears
Conditions that cause abnormal hip movement can also lead to hip labral tears.
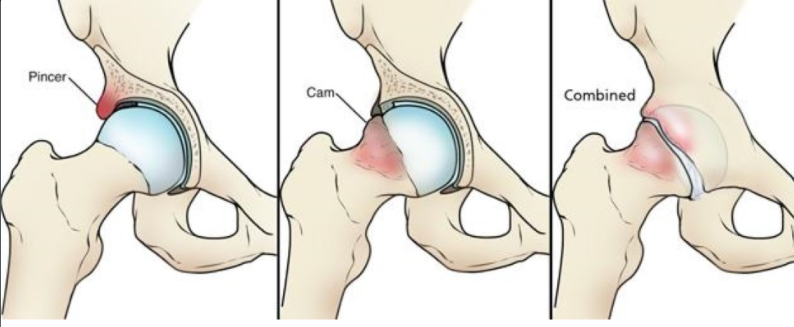
Femoroacetabular impingement (FAI) is a condition where the femoral head does not fit into the socket (acetabulum) properly. This can occur where bones do not form normally during childhood growing years. Excess bone grows around the hip, the additional bone causes abnormal contact between the hip bones and prevents them moving smoothly during activity. This damages the soft tissues during hip movement and due to its abnormal shape causes friction resulting in pain. This poor fit can cause long lasting groin pain and movement limitations. Over time, this can result in tears of the labrum and the breakdown of articular cartilage (osteoarthritis).
There are three types of impingement, Pincer, Cam and a Combined impingement as seen below.
Injury – trauma to the hip can lead to a hip labral tear. Generally, this can happen to people who play sports that have repetitive and high impact movements.
Degenerative health conditions – Osteoarthritis is a chronic (long-term) wearing down of the cartilage between the joints. As cartilage slowly erodes over time, it becomes more prone to tearing.
Symptoms
- Pain often occurs in the groin area. It may be sharp pain when squatting, twisting and turning. Sometimes, the pain is just a dull ache.
- Stiffness
- Limping
Diagnosis of a hip labral tear
Your patient history and a physical examination during a consultation will help Dr Savvoulidis with the diagnosis.
Dr Savvoulidis will conduct the impingement test, where he will bring your knee up towards your chest then rotate it inward towards your opposite shoulder.
Plain x-rays can alert doctors to problems with the hip bones such as (FAI) or osteoarthritis.
Magnetic Resonance Imaging (MRI) – this diagnostic imaging shows a detailed view of the soft tissue surrounding the hip joint. An MRI can show where the labral tear is and how severe it is.
Conservative Treatment
A hip labral tear will not heal on its own, however minor tears can be managed with nonsurgical treatments including:
- Rest and limiting activity to control discomfort.
- NSAIDS – taking non-steroidal anti-inflammatory drugs, such as aspirin or ibuprofen, for a limited time may reduce inflammation and pain in the hip area.
- Injections – Dr Savvoulidis may recommend local anaesthetic fluid injection directly into the hip if the pain has not subsided from other approaches. A steroid may be added to the injection depending upon the level of hip pain and any other existing hip problems.
- Physiotherapy – a physiotherapist can devise an individual treatment plan. The focus of these exercises is to stretch and strengthen the buttocks, thigh, back and the hip muscles aiming to relieve pain whilst also improving hip stability.
If these nonsurgical treatment options fail to relieve symptoms within 10-12 weeks, or if the tear is severe, surgery may be recommended.
Surgical Treatment
Surgery to repair a hip labral tear is usually done arthroscopically. This is a minimally invasive surgery in which Dr Savvoulidis makes small incisions (cuts) in the hip and uses a camera (which displays pictures on a television monitor) to guide miniature surgical instruments to make the following repairs:
- Repair or clean out any damage to the labrum and articular cartilage.
- Debridement (removing a small piece of labral tissue)
- Correct the FAI by trimming the bony rim of the acetabulum and
- Also shaving down the bump on the femoral head.
Arthroscopic surgery cannot always be performed. Bony abnormalities or other hip conditions may make it difficult for Dr Savvoulidis to access the hip joint with an arthroscope. In these cases, or if there is severe damage to the hip this may require open surgery.
Recovery
Recovery and long-term effects of the surgery will depend on many factors, including the type of damage that was present in the hip as well as the patients age. Weight bearing is limited for 4-6 weeks and an individualised rehabilitation program should begin soon after the procedure. You will be seen by the physiotherapist whilst you are in hospital to begin your rehabilitation.
Hip Arthroscopy
We are currently revising our Hip Arthroscopy information. Check back soon, or contact our office for more information
